This article was originally published on Blockchain Review. Thank you for supporting the partners who make SitePoint possible.
Ever wondered about blockchain applications in healthcare? This post will give you a well-rounded introduction to the transformative potential of blockchain and set out the complex interrelated issues that stand in the way of change.
As an important step in becoming a doctor, graduating medical school students swear to some form of the Hippocratic Oath.
One of the vows within that oath is "first, do no harm" or "primum nonnocere."
While most medical professionals live up to this promise on a daily basis, the same cannot be said for the healthcare systems within which they operate.
Despite significant leaps in the medical field, from devices and wearables to genome sequencing and regenerative medicine, individual improvements have not created the fundamental transformation that national healthcare systems require. [1]
Health management and administrative systems remain relatively untouched by technology and regulatory reform and stand ill-equipped to serve the current and future needs of their target populations.
Demographic Stresses
The world is getting older, especially in developed countries, which is placing a significant strain on healthcare systems. According to a 2015 report by the United Nations Department of Economic & Social Affairs [2]:
- Between 2015 and 2030, the group of over-60s will grow by 56%
- In 2015, one in eight people worldwide were aged 60 or over. By 2030, seniors are projected to account for one in six people globally.
- The aging process is most advanced in Europe and Northern America, where more than one in five people are aged 60 or over as of 2015.
- By 2030, the elderly are expected to account for more than 25% of the populations in Europe and Northern America, 20% in Oceania, 17% in Asia and Latin America and the Caribbean, and 6% in Africa.
In the developing world, particularly Sub-Saharan Africa and Asia, future challenges in healthcare will stem from population increases and economic factors rather than aging.
High population growth coupled with a trickle down of innovations is driving a growing middle-class.

With growth coming almost exclusively from emerging nations, the world's middle class is expected to expand by another three billion over the next two decades. [3]
Delivering efficient, sustainable and affordable healthcare to the world's aging population and emerging middle class will become more difficult without profound and substantive changes to national healthcare systems.
While problems are complex, systemic and by no means easily fixed, the vast majority of constraints experienced by healthcare systems can be traced to a single, yet highly corrosive root cause.
Myopic, Outdated & Restrictive Compliance Regulations
The costs, risks and societal sensitivities surrounding healthcare are profound. Due to the sensitive and central role healthcare plays in society, fearful government officials have been scared to make the deep regulatory changes required to reform healthcare.
Officials know they will be punished by the public and politicians more for underregulating — approving a harmful drug, say — than for tightening the approval process, even if doing so delays a useful innovation. - Regina E. Herzlinger
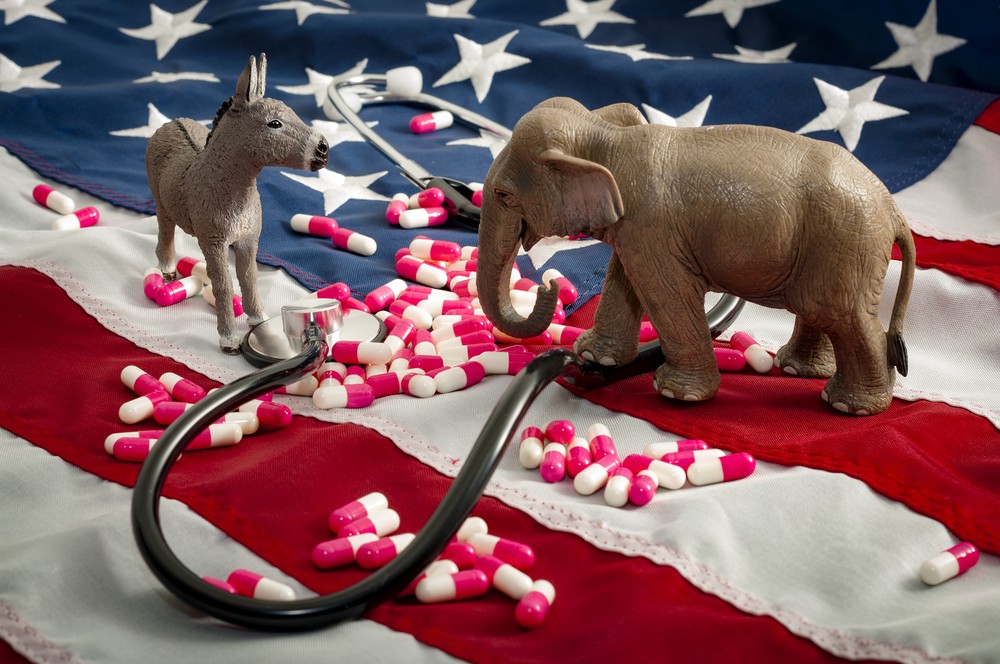
Remember the Obamacare Saga?
Sure you do. It's still going on today, many years later.
The divisive public and congressional debates. The multitude of vested interests and the tangle of regulations. It's not hard to understand why the implementation of far-reaching regulatory reforms have been unattainable and generally avoided by politicians.
Data sharing and privacy laws have resulted in gross inefficiencies, industry-wide fragmentation, and the prevention of real innovation in healthcare. HIPAA, for example, the US Health Insurance Portability and Accountability Act, designed to protect health information, imposes strict rules on healthcare providers.
Despite the Act's noble intention to keep patient data secure and private, it remains a large impediment to efficient patient care mainly because of the difficulties in accessing patient information and restrictions on electronic communications.
Many physicians may be reluctant to embrace EHRs because of malpractice concerns. They may believe that they are better protected against malpractice lawsuits by the handwritten chart system. Furthermore, HIPAA has raised many new issues about data handling. There are also international legal issues about sharing health information. Many unresolved legal concerns surround legal liability in the event of medical errors that are byproducts of health analysis software or EHR data encoding. - A Robust Health Data Infrastructure
Government regulations like HIPAA have caused a host of flow-on problems.
Healthcare management systems designed to adhere to such restrictive regulations are antiquated and fragmented. Bloated systems that run on paper and siloed record-keeping practices have created healthcare management systems that are inefficient, fragmented, isolated and opaque.
The shift towards electronic health records (EHR) has done little to improve the splintered nature of healthcare. A severe lack of interoperability within organizations and at the inter-organizational level means that coordination remains minimal. EHR's are fragmented across hospitals, private practices, labs, pharmacies and many other industry players. [6]
On average, Americans visit 16 different doctors in their lifetime. While both the HITECH and the Affordable Care Act's now enable and in some cases mandate that data from your doctor's visits be stored digitally, medical records and results from different facilities and physicians are often stored in incompatible databases. - Brian Forde
Real-world Implications for Patient Health
The inability to exchange and make use of electronic health records serves as a major impediment to the development of a robust data infrastructure. [8] As you can imagine, when hospitals, clinics, insurers, governments and doctor's offices are unable to share information, this has negative outcomes for patient health.
Einer Elhauge, Founding Director of the Petrie-Flom Center for Health Law Policy, Biotechnology & Bioethics at Harvard writes:
Just as too many cooks can spoil the broth, too many decision makers can spoil health care. Individual decision makers responsible for only one fragment of a relevant set of health care decisions may fail to understand the full picture, may lack the power to take all the appropriate actions given what they know, or may even have affirmative incentives to shift costs onto others. All these forms of fragmentation can lead to bad health care decisions. [9]

Take a look at this example scenario.
A patient seeks medical advice to find a remedy for his constant fatigue and muscle aches.
He/she visits a number of doctors, each a specialist in their respective areas and even visits the hospital on one occasion.
He/she receives a battery of tests from each doctor as well as the hospital and is prescribed a range of drugs.
The patient's condition proceeds to deteriorate, so he/she decides to visit a new doctor who continues a new testing and treatment regime. Throughout the process, the medical professionals treating the patient have little communication and share minimal information on the patient's medical history.
Even though the doctors who treated the patient in this fictitious, albeit credible real-world example may have followed the right medical procedures to treat the problems they were trained to handle, the fragmented nature of the healthcare system resulted in no co-ordination and ultimately substandard patient care.
The incapacity to share vital information led doctors to be unable to see the patient's bigger picture which could have shed further light on the health condition. Information sharing between doctors would likely have resulted in better treatment and a reduction in patient, doctor and insurer costs that accompanied needless treatments.
Information sharing between doctors would likely have resulted in better treatment and a reduction in patient, doctor and insurer costs that accompanied needless treatments.
The corrosive impact of government regulations doesn't end here.
Fragmented, siloed record-keeping practices and systems that lack basic levels of interoperability are responsible for other major problems in healthcare.
There is now a severe lack of advanced data available for clinical and scientific research and economic, behavioral and infrastructure purposes. With little meaningful data, it's difficult for governments and the healthcare industry to see the bigger picture and make informed decisions to improve the quality of patient care.
There is also insufficient insurable data for the most at-risk and underserved citizens and the tracking of population health trends. [10]
Perhaps the most destructive impact of fragmentation and the inability to share information is that it has caused deep inefficiencies. Healthcare costs, in the United States, for example, have spiraled out of control.
According to the CDC, health expenditures as a percentage of GDP have risen some 4.5% since the year 2000. [11]
Health expenditures % of GDP:
- 2000: 13.3%
- 2009: 17.3%
- 2014: 17.4%
- 2015: 17.8%
High costs have contributed to insurance companies' reluctance to insure the population and provide an adequate range of services.
Many national healthcare systems are so inefficient they have become unable to deliver any form of care to the most vulnerable and at-risk members of society. Many are even failing to deliver adequate care to those that can afford it.
As demographic shifts take place, these inefficiencies will worsen. The reinvention of the national healthcare systems is now required.
Blockchain technology is a key tool to achieve healthcare objectives for developing and "re-developing" nations.

One of the fundamental goals that governments and industry seek to achieve is to provide improved quality of healthcare at lower healthcare costs. [12] Making this goal a reality will require governments and industry to play different, but equally important roles.
Governments: must lead change through regulatory reforms that incorporate technological advances and foster an environment designed around competitive collaboration and innovation amongst insurers, healthcare providers, and regulators. It's equally imperative for governments to participate in technological innovation programs and R&D to support the development of a robust health data infrastructure.
It's equally imperative for governments to participate in technological innovation programs and R&D to support the development of a robust health data infrastructure.
Industry: Transforming the
Continue reading %How Blockchain Can Help Re-invent Healthcare%
by Anthony Back via SitePoint
No comments:
Post a Comment